Snoring & Sleep Apnea – Powell, OH •
Learn More So You Can Sleep Better
A full night’s sleep is essential to your overall health. If you are well rested, you will feel good and be able to function at your best. According to statistics, approximately 25 million adults in the United States suffer from obstructive sleep apnea (OSA), and more than three times that number snore! At our office, we provide care to address these issues so that you can enjoy a safe and uninterrupted night’s sleep.
Why Choose Powell Dental Sleep Solutions for Snoring & Sleep Apnea Treatment?
- Multiple treatment options under one roof
- Custom-made sleep appliances
- Quadruple board-certified doctor
What Is Sleep Apnea?

When a person has sleep apnea, they experience repeated pauses in breathing while asleep. This causes the body to go into “panic mode” and partially wake up to restore breathing, preventing someone from getting the deep, restful sleep they need to feel energized throughout the day. This is most often caused by the soft tissues in the mouth and throat relaxing into and blocking the airway, which is called obstructive sleep apnea (OSA). These kinds of blockages can occur up to 100 times per hour, and in many cases, patients wake up completely unaware that they have occurred (though some wake up gasping or out of breath).
How Does Snoring Develop into Sleep Apnea?

The sound of snoring is produced from the upper airway of your throat and caused by loose and relaxed vibrating tissues during breathing. The sound may come from the soft palate and uvula, the back of the throat and tongue, or a combination. It is an indication that air is having difficulty passing through the airway. It may also be a sign that the person has an upper airway resistance or constriction, indicating a serious health condition called obstructive sleep apnea (OSA). About 50% of snorers have OSA. It is possible that some persons may have OSA and not snore. Snoring is considered a precursor to Upper Airway Resistance Syndrome (UARS) and can often progress into Obstructive Sleep Apnea (OSA).
What Causes Sleep Apnea?

The causes of sleep apnea are many, which is why it’s important for you to undergo extensive testing to determine the underlying reason for your inability to breathe freely and get adequate rest. Your symptoms will likely place you in one of two categories: obstructive sleep apnea (OSA) or central sleep apnea (CSA), which can help determine which type of treatment you need to experience effective results. However, before that can be determined, we must establish the root cause of your sleep problems, which can include:
Sleeping Position

Obstructive sleep apnea (OSA) is the most common form, so if you struggle with sleep interruptions throughout the night, it may be because of your sleep position. When lying on your back, the tongue or soft tissues can easily fall back onto your throat, causing a blocked airway. Instead, try sleeping on your side or stomach, as this will reduce the chances of ceased breathing; instead, allowing for an unobstructed airway.
Excess Weight

If you are overweight or obese, the chances of developing sleep apnea significantly increase. As fat accumulates in areas of the body, specifically around the neck, it can create a narrower airway, making it easier for a blockage to occur. By sticking to a weight loss regimen of regular exercise and eating nutrient-rich foods, you can lose excessive body weight and improve your sleep apnea symptoms.
High Blood Pressure

Lack of airflow can have a serious effect on your overall health and well-being, especially if your oxygen levels are continually rising and lowering throughout the night. Each time you stop breathing, your brain must be triggered to wake you up. This causes your blood vessels to tighten, which can lead to hypertension. Regulating your blood pressure is essential, and it can be improved by seeking sleep apnea treatment.
Alcohol & Tobacco Use

Ending the evening with an alcoholic beverage to “decompress” after a hard day can be harmful to your sleep habits. Alcohol is known to work in the same way as a sedative. When falling asleep, your throat muscles begin to relax, causing them to fall back onto your airway, creating an obstruction. Smoking and tobacco use can be just as harmful because of the inflammation that occurs in the airway when inhaling nicotine. Finding ways to kick your alcohol and tobacco habits will prove beneficial when looking to improve your sleep and overall health.
Family History

Oftentimes, sleep apnea can be attributed to family genetics. If you have a parent, grandparent, or another family member who suffers from sleep apnea, there is an increased chance that you will, too. Based on the structural design of your airway and face, you may find it harder to breathe freely while sleeping. Meeting with a skilled sleep dentist can help you determine how best to address this genetic problem.
What Are Some of The Signs & Symptoms of Sleep Apnea?

Knowing if you might be suffering from sleep apnea isn’t always easy. For individuals with a partner who can express concern because of loud snoring or frequent episodes of ceased breathing, it typically does not take as long to achieve a formal diagnosis. However, if you live alone or do not know the various signs and symptoms that come with this common sleep disorder, our team is here to help. With nearly 20 million people in the United States suffering from some form of sleep apnea, we believe the list provided below can help you to better identify problems you might be experiencing and, in turn, seek professional help to get the treatment you need.
Loud Snoring

There is a common misconception that if you snore, you have sleep apnea and vice versa. Yes, snoring is a common factor when it comes to diagnosing a sleep disorder but yours may only be due to sinus congestion or another external factor. However, if your snoring is loud and persistent, there is a good chance you have some form of sleep apnea. This type of snoring occurs when the throat collapses, causing your air passage to become narrow.
Chronic Fatigue

It should come as no surprise that sleep apnea causes chronic fatigue. When you are frequently interrupted as a result of your inability to breathe throughout the night, you will be unable to complete the full sleep cycle and wake feeling tired and groggy. As a result, this can negatively impact your personal and professional life.
Morning Headaches/Sore Throat

A headache at any time of day is troublesome; however, one that occurs when you first wake up can set a negative tone for the rest of your day. With sleep apnea, specifically OSA, carbon dioxide can cause your brain’s arteries to dilate when regular breathing does not occur. As pressure builds inside the skull, it can lead to a painful and bothersome headache when you wake up.
Memory Loss

You may not realize it but part of the sleep cycle that is necessary to function each day includes storing memories. Whether it was completing part of a project at work or watching your daughter at her dance recital, these are experiences your brain works to store while you’re sleeping. If sleep apnea prevents you from completing your sleep cycle, it becomes much harder to develop new memories, causing you to become more forgetful.
Inability to Focus

If you struggle with insomnia as a result of your sleep apnea, you may notice a difference in your ability to focus on a particular task. This can have serious consequences when it comes to work and/or school. If the brain cannot identify which distractions should be avoided because of a lack of sleep, it is likely you are spending more time on your phone or reading a news article at your company than devoting time to your work or school assignments.
Mood Regulation/Depression

When you are unable to get the sleep you need because you cannot breathe properly, it will impact other areas of your life. Whether you no longer function at work like you used to or your relationships are suffering, these changes can ultimately affect your mood and lead to depression.
Gasping for Air/Out of Breath

One of the clear indicators that you need to see a sleep dentist is gasping for air or being out of breath when you wake throughout the night. Because of the collapse that occurs inside your oral cavity, a blockage forms, making it impossible for air to flow freely. Should you stop breathing, your body will be triggered by the brain to wake, causing you to gasp or feel out of breath.
Weight Gain/Weight Loss

It’s not uncommon to experience weight gain or weight loss while dealing with sleep apnea. Hormonal changes can occur when dealing with lack of sleep, causing your metabolism to work differently than before. If you find it hard to go back to sleep when waking from an apnea episode, you may turn to food, which can lead to weight gain and greater fat deposits around your neck.
Low Libido

When you’re constantly tired because you cannot achieve adequate rest, it’s highly unlikely you’ll be ready to engage in any sexual activity. Of course, it’s not just fatigue that causes both men and women to lack the desire for intimacy. Researchers have discovered that sexual dysfunction and loss of libido are quite common among those who suffer from serious cases of sleep apnea.
Bruxism (Teeth Grinding)

It is believed that some patients who suffer from sleep apnea also experience problems associated with bruxism. Also known as teeth grinding or clenching, this can occur as a response to your body’s sudden awakening when triggered to breathe throughout the night. Because the brain must alert the body, it can cause a stress response that, in turn, causes you to grind your teeth.
High Blood Pressure

Obstructive sleep apnea (OSA) is most commonly associated with high blood pressure. Because individuals with OSA can have one or hundreds of apnea episodes each night, the frequent waking causes blood pressure to rise and fall over and over again. As the heart becomes more strained due to a lack of sleep, the nervous system will cause the body to experience greater stress (i.e., faster heart rate, high blood pressure, etc.). As a result, this can lead to the development of cardiovascular disease.
The Consequences of Sleep Apnea
Chronic fatigue and sleepless nights are not the only negative side effects that can occur when living with sleep apnea. Researchers have spent years looking at the connection between sleep and how it impacts a person’s overall health. As you think about the problems you are experiencing and how they are affecting your daily routine and life, take some time to consider the consequences of sleep apnea in Powell.
Mental Health

Lack of sleep doesn’t just make you sleepy. It can also cause you to become irritable, depressed, anxious, and even angry toward others. Over time, this recurrence can take a toll on your mental health and lead to cognitive decline. It’s no surprise that many patients with untreated sleep apnea begin to experience memory loss and the ability to focus – both of which can impact a person’s personal and professional life.
Digestive Health

If you are unable to breathe properly and sleep without interruptions each night, you may notice problems associated with your digestive health. Acid reflux, heartburn, and even abnormal liver function (inability to digest fats and nutrients) can all become increasingly challenging the longer you go without sleep apnea treatment. It can become a vicious cycle – one that you cannot be relieved from unless you seek professional care.
Immunity

If you have sleep apnea and have not yet sought treatment for it, you may be putting yourself at risk when it comes to preventing colds, infections, viruses, and other diseases. A healthy immune system helps prevent these problems; however, if your body is unable to get the rest it needs to re-energize and remain healthy, frequent illnesses may begin to impact your ability to do your job, maintain positive relationships, and enjoy a better quality of life.
Insulin Levels, Diabetes, and Metabolic Syndrome

High blood pressure, diabetes, insulin resistance, obesity, and high cholesterol are all potential risk factors associated with untreated sleep apnea in Powell. Chronic fatigue may cause you to feel too tired to exercise or eat right, resulting in weight gain and unhealthy habits. Over time, if you develop diabetes or any of these other problems, you may find it harder to get your blood glucose levels and overall health under control.
Respiratory System

Obstructions that occur throughout the night can make it nearly impossible for air to flow freely. The frequency with which this happens can negatively affect your respiratory system, even increasing your risk of developing asthma. Seeking professional help to prevent obstructions so that you can breathe freely throughout the night is essential if you want your lungs to function properly.
Bodyweight

Sleep apnea and obesity are closely linked. When too much weight exists around the waist and/or neck, it increases the chances of sleep apnea. But your rest will not be the only thing affected. Excessive fat and frequent, nightly interruptions caused by your inability to breathe can cause additional strain on your heart, leading to stroke, heart attack, and other cardiovascular problems.
Cardiac Health

Each time you stop breathing at night, your brain must alert your body. This can cause your heart rate to increase, initiating what might feel like a stage of panic. When you wake up, you may begin gasping for air. If this happens multiple times while you are asleep, you may develop poor heart health. Not only will your cholesterol (LDL levels) likely be higher, but your blood pressure will remain unstable, and you might experience an abnormal heart rhythm.
How Can I Know If I Have Sleep Apnea?

Most of the time, it’s a bed partner or family member that first notices the stoppages in breathing typically associated with sleep apnea. When a patient goes to see a doctor about this problem, they will recommend that they undergo a sleep study to determine the root cause of the issue. This will involve the patient sleeping while wearing a medical device to monitor their vital signs. After the study has concluded (which only involves one night of sleep), the results will be evaluated by a sleep doctor, who can then determine whether or not a patient has sleep apnea.
What Is AHI?
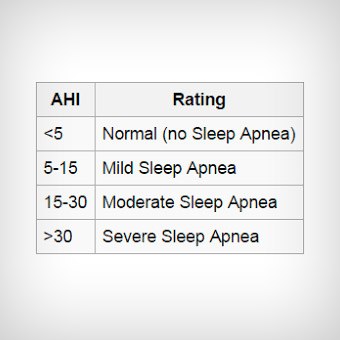
This acronym represents a summarized measurement for types of breathing obstructions that meet certain criteria.
- The ‘A’ represents ‘apnea,’ which means without breath or oxygen delivery for 10 seconds or longer.
- The ‘H’ represents ‘hypopnea,’ which refers to abnormally slow or shallow breathing for 10 seconds or longer and a drop-in oxygenation by 4% or greater.
- The ‘I’ indicates an ‘index’ that can be thought of like an overnight hourly average. It is calculated by adding the total number of apneas plus hypopneas and dividing that number by the total amount of hours slept to obtain the AHI.
“RERA’s” are sleep disordered breathing events that do not qualify as an apnea or hypopnea. They can fragment sleep and can cause poor sleep quality and inflammation, however, they are not counted within the AHI calculation. They may be calculated in a separate respiratory index report.
How AHI Relates to Sleep Apnea

An AHI between 0-4.9 events/hour is classified as normal, although these persons may have respiratory disturbance events that cause symptoms seen in OSA. Mild sleep apnea is an AHI of 5.0 to 14.9 events/hour, moderate is greater than or equal to 15 but less than 30 events/hour, and severe sleep apnea is greater than or equal to 30 events per hour.
Subtle breathing irregularities may briefly block the airway and cause your sleep to be interrupted. These respiratory events are included with the apnea and hypopnea events in the RDI (respiratory index) measurement, therefore the RDI may be higher than the AHI.
Oxygenation, Sleep, and Why It Matters

For a healthy person, a normal blood-oxygen saturation is between 96-99% at sea level. At night, our respiratory effort decreases, and oxygenation will dip lower than when awake. While small reductions are normal, those with sleep apnea can experience a drop in oxygenation that has many negative health effects. Reduction to not less than 90% is considered mild. However, dips into the 80-89% range are considered moderate, and those below 80% are severe.
When the body is deprived of oxygen, the heart rate and blood pressure increases, placing stress on the heart from activation of the nervous system. Chemicals are released into the blood that cause inflammation and promote elevations in blood sugar. This inflammation can damage the heart, kidneys, brain, and blood vessels, increasing the risk of heart disease, stroke, and obesity.
A sleep study can reveal the levels of oxygenation during your sleep. Additionally, it can give us clues as to how sleep deprivation and fragmentation may adversely affect your brain health, memory consolidation, and overall feelings of vitality.
The Different Types of Sleep Apnea

When meeting with your sleep dentist to discuss your symptoms and inability to get the rest you need, one of the first steps is identifying which type of sleep apnea you have. Not everyone suffers from the same version but instead will exhibit signs related to one of the following: obstructive, central, or mixed sleep apnea. Keep reading to learn more about each kind and how your sleep physician can determine which one you have based on a sleep study.
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) occurs when the muscles in the back of the throat collapse onto the airway, causing it to become repeatedly blocked. This can cause you to experience interrupted sleep, as you wake choking or gasping for air. OSA commonly occurs in individuals who are older and have weaker throat muscles, those who smoke or drink alcohol excessively, and those who are obese. Also, having enlarged tonsils can contribute to OSA.
Learn More About Obstructive sleep apnea (OSA)
Central Sleep Apnea
Central sleep apnea (CSA) occurs when the respiratory center in the brainstem does not activate properly to alert the patient to breathe. This type of sleep apnea can also cause you to wake up gasping for air. You may find that if you have any of the following, you may be more prone to CSA than any other form of sleep apnea:
- You have congestive heart failure or an irregular heartbeat
- You are over the age of 60
- You have a brain condition (i.e., stroke, brain tumor)
- You take certain medications, specifically opioids
Mixed Sleep Apnea
Mixed sleep apnea is a combination of obstructive and central sleep apnea. This tends to occur when the airway becomes blocked while experiencing central sleep apnea. When it comes to treating mixed sleep apnea, it’s not uncommon for a CPAP machine to be recommended; however, there is also the option of incorporating an oral appliance as well.
Dangers of Sleep Apnea

While you might think the only negative aspects of sleep apnea are the loud snoring that bothers your partner and feeling fatigued while at work, these are only a small fraction. The truth is that untreated sleep apnea can have a devastating effect on your overall health, ability to function behind the wheel, and personal and professional relationships. Both short- and long-term consequences can develop if remain unchecked. It’s important to identify the dangers associated with sleep apnea so that you can get the help you need before it becomes a serious problem for you and those around you.
Short-Term Consequences

When thinking about the short-term consequences associated with sleep apnea, chronic fatigue is likely to be at the top of the list. Waking up and being unable to function at your best can lead to less production at work and, more devastatingly, the potential for a serious accident. Attempting to get behind the wheel of a vehicle while drowsy puts you and others on the road at risk.
The National Highway Traffic Safety Administration states that in 2017, more than 91,000 drowsy driving crashes occurred. With nearly 800 deaths occurring, it’s imperative that seeking treatment for sleep apnea can save your life or the life of someone else.
Long-Term Consequences
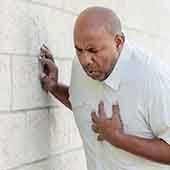
Sleep apnea doesn’t just affect your inability to complete your work or drive a car, but it can take a toll on your overall health and well-being. Whether it is feeling more depressed or anxious, struggling to remember certain things, or experiencing fast weight gain, your body and brain will become negatively impacted.
Also, it is not uncommon for those with sleep apnea to develop high blood pressure. This, in turn, can lead to an increased risk of heart attack and stroke. These damaging effects, over time, will only worsen if sleep apnea is left untreated.
Those who struggle with obesity or are overweight are already at risk for sleep apnea, but the inability to gain control over one’s sleep will more than likely increase their chances of gaining more weight. When feeling tired all the time, the desire to exercise and eat right is suppressed because of the hormonal imbalance that can occur.
How Sleep Apnea Affects Relationships

Snoring is known to be a common symptom of sleep apnea. If you live alone, this may not be an issue; however, when sharing a bed, you may find that your partner becomes frustrated because of the loud snoring. This can lead to bickering and arguing due to a lack of sleep for both of you. Not to mention, they might start sleeping in another room, which can create even bigger problems.
Getting treatment for sleep apnea is the most effective way to keep everyone in your household happier and less irritable, including yourself. It should also be a clear indicator of how serious sleep apnea really is if you seem to always be at odds with those you love.
Don’t wait any longer to seek professional help for your sleep apnea. The team at our office is here to help!
What Is the Treatment for Sleep Apnea?

As we touched on above, there are various types of sleep apnea, and the specific type or combination of types determines the treatment options available to a patient. The most common and gold standard treatment for OSA is positive airway pressure treatment (PAP), which may be referred to as CPAP, Bi-PAP or Auto-PAP. They all work by delivering pressurized air through a nasal or face mask to keep the airway open throughout the night.
In cases of mild or moderate obstructive sleep apnea, an oral appliance can be designed to advance the lower jaw and keep the tongue and soft tissues in the back of the throat from collapsing, thereby enabling the airway to remain open while sleeping. These appliances are easy to wear, easy to care for, and are comfortable as well as portable.
In cases where a patient is PAP intolerant, an oral appliance can serve as a viable alternative. In 2015, the American Academy of Sleep Medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM) updated treatment guidelines and recommendations for oral appliance therapy versus CPAP therapy.
 In summary, they said that either oral appliance therapy (OAT), CPAP therapy, or InspireUAS therapy can be considered as appropriate first-line treatments for upper airway resistance or mild to moderate obstructive sleep apnea and snoring. This suggests that either may be offered as an effective therapy based on a patient’s preference, although PAP therapy is still recognized as the gold standard. Oral appliance therapy should be considered as an appropriate first line option for patients with mild to moderate obstructive sleep apnea and snoring, or if a patient refuses, is intolerant, or finds CPAP therapy ineffective, even if severe.
In summary, they said that either oral appliance therapy (OAT), CPAP therapy, or InspireUAS therapy can be considered as appropriate first-line treatments for upper airway resistance or mild to moderate obstructive sleep apnea and snoring. This suggests that either may be offered as an effective therapy based on a patient’s preference, although PAP therapy is still recognized as the gold standard. Oral appliance therapy should be considered as an appropriate first line option for patients with mild to moderate obstructive sleep apnea and snoring, or if a patient refuses, is intolerant, or finds CPAP therapy ineffective, even if severe.
And, if neither of these options are effective, corrective surgery is another available treatment. This is normally used only if a patient has a physical obstruction in their airway, such as a deviated septum or a large set of tonsils, adenoids, or a bigger than average uvula.
Understanding the Cost of Sleep Apnea Treatment

At our office, our team of experts understands that the financial responsibility of sleep apnea treatment can be overwhelming. Because of the many tests and treatment options that must be completed, it’s natural to have questions about how much it will cost you out of pocket. Fortunately, our sleep team is ready to work with you to navigate these financial waters. We’ll go over your medical insurance information and determine the best way to get you the care you need at a price you can afford.
Does Dental Insurance Cover the Cost of Sleep Apnea Treatment?

No. Most dental insurance companies will not cover the cost of sleep apnea treatment because it is commonly viewed as a medical issue that requires medical devices to treat. Each plan is different though, so it’s important that you allow us to review your plan first.
Factors That Affect the Cost of Sleep Apnea Treatment

When it comes to determining how much your treatment will cost, there are various factors that Dr. Shults and our team must consider, such as:
- The type of sleep apnea treatment you choose to move forward with (i.e., oral appliance therapy, CPAP, Bi-PAP, etc.)
- How much you are willing to pay out of pocket for treatment
- The severity of your sleep apnea/snoring
Our team will go over all of these details with you during your consultation. This will help to eliminate any surprises before moving ahead with treatment. We will make sure to complete the appropriate paperwork so that you have a clear understanding of your financial obligations once a claim is filed with your medical insurance company.
Treat Your Sleep Apnea Now to Improve Your Health

If you want to avoid costlier health-related conditions that can worsen as a result of untreated sleep apnea, it’s best to go ahead and seek professional care right now. Continual obstructions can lead to strokes, heart attacks, cardiovascular disease, diabetes, depression, and more.
It is believed that billions of dollars are spent on treating chronic health conditions that may be avoidable if sleep apnea symptoms were properly addressed. Taking care of your sleep health now can save you thousands of dollars (or more) in the long run because of the positive impact it can have on your physical and mental health.
Making Sleep Apnea Treatment More Affordable

If you’re uninsured and don’t know how you will pay for your sleep apnea treatment, do not neglect it altogether. Instead, ask our team about flexible financing through CareCredit. This third-party financier makes it easy to enroll in low-to-no-interest payment plans. You can sign up with the help of our trusted team of professionals who can help you stay within your budget.
Sleep Apnea FAQs
Living with sleep apnea can take its toll on your physical, mental, and emotional well-being. Without adequate rest, you run the risk of developing serious health problems as well as driving drowsy or suffering the repercussions should it impact your ability to work effectively. Many patients who struggle with this condition have many questions, and our team is here to help. We encourage you to review the information below and call us with any additional questions.
Why should I see a dentist for sleep apnea treatment?
Although it might seem odd to leave your treatment up to a dental professional, the fact is that these experts are well-versed in problems concerning the upper respiratory area. With obstructive sleep apnea (OSA), the tissues of your neck and mouth can make it difficult to breathe freely. Dentists can reposition your lower jaw so that the tissues do not collapse and block your airway. By choosing to meet with your dentist regularly, you can have a built-in appointment that is focused solely on any issues you are having with your sleep patterns.
Can I diagnose sleep apnea on my own?
Just because you exhibit some of the symptoms associated with sleep apnea does not mean that you have it. They are commonly found in other issues, which is why it’s important that you seek treatment from our trusted professionals. This will ensure that you receive a proper diagnosis. While various technologically advanced health aids (i.e., an Apple watch) can help, they do not test strictly for sleep apnea. Also, you must undergo a sleep test in order to receive a formal diagnosis, so you’ll need to visit a sleep doctor.
Will my sleep apnea go away if I lose weight?
There is a possibility that you will begin to sleep better if you lose weight. The reason for this is that obesity and being overweight are considered risk factors for OSA. If you have excess weight and tissue, especially around your neck, it can block your airway, making it difficult to breathe. By losing unwanted pounds, you can reduce the amount of excess tissue in this area and improve the flow of oxygen through your airway. But it’s important to remember that even if you lose weight, you might still experience sleep apnea. This is why a sleep test is important to determine if you still have it.
Can I have oral appliance therapy if I grind my teeth?
Yes, you can undergo oral appliance therapy even if you grind your teeth. These devices are designed to withstand the pressure of teeth grinding, and they can help minimize the potential for tooth damage caused by bruxism. It is not uncommon for both teeth grinding and sleep apnea to go hand in hand, so wearing a customized oral appliance will help to improve both while undergoing treatment.
